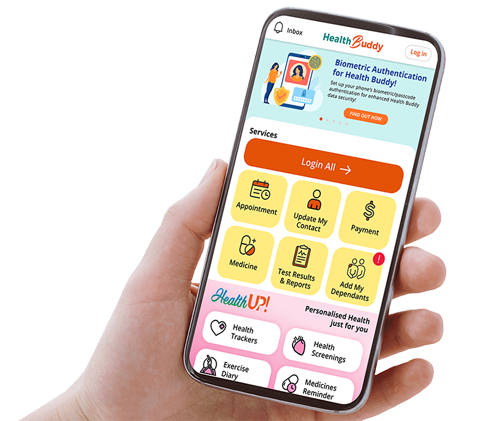
E-services such as appointments, payments will not be available from 10pm 6 Sep (Sat) to 10am 7 Sep (Sun) due to maintenance on HealthHub.
Beware of fake advertisements on social media using the SGH logo to promote products. SGH does NOT promote, advertise, or endorse any particular brand or product in accordance with the Healthcare Services Act. Stay vigilant and ignore these fake advertisements.
 The CGH care team at SCAC provides aeromedical screening and aviation physiology training for the RSAF.
The CGH care team at SCAC provides aeromedical screening and aviation physiology training for the RSAF.
At altitudes of nearly 10,000m above sea level — where the air is thin and regular flights can affect the human body in complex ways — aviation medicine plays a crucial role in safeguarding the health and lives of pilots and passengers. This specialised field, that bridges the realms of healthcare and aeronautics, extends far beyond the confines of an aircraft cabin. It ranges from ensuring a pilot’s fitness to command a plane carrying hundreds of lives, to training military aviators to navigate the physical demands of their planes.
AVIATION MEDICINE focuses on the health, safety and performance of individuals involved in aviation to ensure safe operations. These individuals include pilots, air traffic controllers and aircrew, as well as passengers and airport ground support personnel.
Aviation medicine has long been a part of CGH’s legacy of care, with its roots dating back to 1935 when the old British Royal Air Force Hospital was built in Changi. This foundation laid the groundwork for what would become a centre of excellence in aviation medicine.
In 1975, the hospital further served Singapore Armed Forces (SAF) personnel and their families under the name, the UK Military Hospital. That same year, the hospital began offering essential medical care, including accident and emergency services, as well as general and dental surgery to the public.
The first aviation medicine centre in Singapore
It was a pivotal moment in Singapore's aviation medicine landscape when CGH set up the first aviation medicine centre within a restructured hospital with the Civil Aviation Authority of Singapore (CAAS) in June 2019.
Today, the Changi Aviation Medicine Centre (CAMC) serves as a hub for civil and military aeromedical services as well as aviation physiology training.
“CGH is the first public healthcare institution to establish an aviation medicine service through the CAMC, bringing this clinical specialty into mainstream healthcare, and supporting the holistic health and wellbeing of our pilots and air traffic controllers. This opens new possibilities for collaboration and innovation with the aviation industry,” says Clinical Professor Ng Kee Chong, Chief Executive Officer, CGH. Together with CAAS and the Republic of Singapore Air Force (RSAF), CGH will advance aircrew healthcare, aeromedical research and innovation, and specialist training to elevate aeromedical excellence.
 The CAMEC provides comprehensive specialist healthcare services and clinical support for aviation professionals.
The CAMEC provides comprehensive specialist healthcare services and clinical support for aviation professionals.
At CAMC, aviation professionals have access to comprehensive clinical specialist services delivered by a multidisciplinary care team, along with access to imaging, laboratory and other clinical support facilities available at CGH. By combining evidence-based treatments with aviation-specific medical expertise, CAMC ensures all prescribed treatments are compatible with aerospace medical requirements.
CAMC started its services at the Civil Aviation Medical Examination Centre (CAMEC) in July 2020. This facility provides civil aviation licence holders with improved medical support and greater convenience by offering medical fitness assessments, licence renewals and collection services in one location.
Supporting the Republic of Singapore Air Force
To continue pushing the frontiers of aeromedical research and ensure that aviation professionals receive the highest standards of medical care, CGH partnered the RSAF to establish the Singapore Changi Aeromedical Centre (SCAC) in February 2025. A Memorandum of Understanding was signed to jointly establish a regional Centre of Excellence in Aviation Medicine.
The SCAC is a one-stop centre that provides aeromedical services encompassing clinical screening and aviation physiology training for RSAF aircrew and other commercial clients, helping to enhance military aircrew health and performance through fitness-to-fly assessments, aeromedical evaluation protocols and operational aviation physiology training.
“Through these centres, CGH has established itself as the largest aviation medicine practitioner in Singapore, ensuring safe aircraft operation and control capabilities for both military and civil aviation,” says Dr Robin Low, Head and Senior Consultant, Occupational and Aviation Medicine Service, CGH.
“CGH is also accredited by the Singapore Joint Committee for Specialist Training as a site for the Aviation Medicine Sub-Specialty Training Programme. Beyond Singapore, the CAMC is attracting interest from overseas air forces and aviation institutions seeking aeromedical expertise.”
 Clinical Professor Ng Kee Chong, CEO,
Clinical Professor Ng Kee Chong, CEO,
CGH; and Mr Han Kok Juan, Director-General, CAAS.
ENHANCING MENTAL HEALTH AND WELLNESS SUPPORT
As part of a comprehensive strategy to enhance aviation safety, CAAS and CGH are expanding their collaboration in the domain of mental health and wellness support, to address the unique psychological demands faced by aviation professionals across the sector. Building on more than seven years of strategic partnership, CGH and CAAS inked a Collaboration Agreement that brings together CGH’s clinical expertise with CAAS’ industry knowledge to develop specialised mental wellness programmes and resources for the aviation community.
“As Singapore’s leading aviation medicine practitioner and a regional centre of excellence, CGH is committed to caring for, and supporting the health and wellness of our aviation professionals in this sector,” says Clinical Professor Ng Kee Chong.
Mr Han Kok Juan, Director-General, CAAS, adds: “The CAAS-CGH partnership allows us to identify and address the needs of these professionals in a more targeted manner, taking into consideration their unique operating environment and the psychological demands of their work.”
The Flight Plan
Pilots first undergo detailed health checks by the CGH care team to ensure they are medically fit for flying duties
At the heart of aviation medicine lies the critical task of ensuring that aircrew are prepared for the unique challenges of flight. Pilots need to be medically fit before earning the right to fly. CGH’s rigorous medical assessments in line with international and local regulations certify this. These licensing and certification examinations ensure that every pilot who takes to the skies can operate and control the aircraft safely.
 CGH Clinic Assistant Nur Rabiatul Adawiyah Binte Abdul Jalil conducts audiometry tests for individuals according to aviation requirements.
CGH Clinic Assistant Nur Rabiatul Adawiyah Binte Abdul Jalil conducts audiometry tests for individuals according to aviation requirements.
Giving the all-clear
Good hearing and vision are essential for pilots to communicate with other aircraft or air traffic control. Clear hearing enables pilots to receive and understand crucial radio communications that could affect flight safety and navigation. While radar and automated landing systems have become commonplace, good vision remains critical to pilots’ ability to spot other aircraft, read their instruments and flight charts, and to land safely.
At the CAMEC, civil pilots undergo a comprehensive battery of tests according to their age and in line with CAAS’s requirements. These include haemoglobin, cholesterol and glucose tests, electrocardiograms (ECG), audiometry and a range of detailed eye tests used to assess colour vision. Military pilots undergo a similar battery of tests, but the requirements are more stringent due to the demanding nature of military operational flying. For example, military pilots need to fit within a narrow range of anthropometric measurements — not only height and weight, but also arm reach, sitting height and thigh lengths, among others. This is to ensure that the pilot can fit within an aircraft equipped with an ejection seat, which is activated during an emergency egress.
 Beyond performing licensing and certification examinations for aircrew, Dr Alvin Woo manages their clinical cases that could impact flight safety.
Beyond performing licensing and certification examinations for aircrew, Dr Alvin Woo manages their clinical cases that could impact flight safety.
Dr Alvin Woo, Associate Consultant, Occupational and Aviation Medicine Service, CGH, emphasises that pilots’ and aircrew’s medical fitness is crucial, as it affects both their own safety, and that of passengers and the public. “Our comprehensive evaluations ensure aircrew are physically and mentally fit to operate sophisticated aircraft systems. ” Says Dr Woo. “This work is a crucial component of accident prevention and maintaining operational readiness across both commercial aviation and military operations.”
[IMAGE]
CGH Senior Radiographer Teo Shi Yun performs a chest X-ray, which is required as part of checks for civil and RSAF pilots.
Besides aviation medicine specialists, the multidisciplinary team includes nurse clinicians, radiographers and optometrists, who support the screenings for aspiring pilots and RSAF servicemen and women.
Nurses play a vital role in patient education and knowledge-sharing, enabling and empowering patients to gain better insights into their health conditions. This understanding is particularly crucial for aviation professionals, including pilots and air traffic controllers, as it helps them maintain their fitness to perform their duties.
 CGH Senior Staff Nurse Samuel Tay conducting a stress ECG that assesses heart functions under physical stress.
CGH Senior Staff Nurse Samuel Tay conducting a stress ECG that assesses heart functions under physical stress.
“It is not uncommon to discover some medical conditions in our patients through the various blood tests,” shares Samuel Tay, Senior Staff Nurse, SCAC, CGH. “By educating them on their condition, I help them better understand and manage their health. The knowledge provided also helps alleviate their concerns about how health issues might affect their long-term ability to fly or control aircraft.”
Providing comprehensive care
Pilots occasionally encounter different health challenges, ranging from cardiovascular issues, fatigue and musculoskeletal problems to mental health concerns. In addition to certifying a pilot’s fitness to fly, CGH’s aviation medicine specialists play a key role in helping aircrew navigate medical conditions that may affect their flight safety.
Tapping on the multidisciplinary expertise within CGH, aviation medicine specialists collaborate with specialists across multiple disciplines such as cardiologists, ophthalmologists and psychiatrists to provide comprehensive care while maintaining aviation safety standards. Doctors at CAMEC and SCAC can refer pilots recovering from pneumothorax to lung specialists at CGH, while those with musculoskeletal conditions, such as backache, can be referred for sports medicine consultation and treatment. “Early detection and treatment of conditions such as hypertension or sleep disorders allows us to implement appropriate monitoring protocols, ensuring pilots can continue their flying duties safely,” adds Dr Woo.
Furthermore, with access to sports medicine specialists and endocrinologists, comprehensive preventive health programmes can be developed for pilots. The CGH care team strives to help pilots maintain their fitness levels, reduce the risk of chronic diseases and injuries, extend their flying careers, and enhance their performance during duty.
“This partnership is important, as it taps on the expertise from both RSAF and CGH, to achieve the common goal of becoming a regional Centre of Excellence in Aviation Medicine,” shares LTC(DR) Aaron Chua, Aviation Medical Officer, Air Force Medical Service, RSAF. “CGH’s provision of clinical services and training to RSAF personnel has enabled RSAF Aviation Medicine Specialists to focus on operationally relevant aeromedical support functions. The RSAF also leverages CGH’s medical capabilities in aviation medicine, medical evidence and clinical best practices to deliver quality aeromedical support to RSAF personnel.”
Training to Fly
CGH’s multidisciplinary team works closely with RSAF aviation medicine specialists to conduct physiology training to prepare military pilots for challenging flight conditions.
The clinical services provided by SCAC work hand in hand with its specialised training. While medical assessments ensure aviation personnel meet the stringent health requirements for flying, the centre’s advanced simulation equipment allows RSAF pilots and aircrew to experience and prepare for various flight conditions and scenarios.
 Pilots undergoing hypobaric chamber training to recognise symptoms caused by insufficient oxygen at high altitudes.
Pilots undergoing hypobaric chamber training to recognise symptoms caused by insufficient oxygen at high altitudes.
The Human Training Centrifuge (HTC) is used to subject the pilot seated inside the machine to high acceleration (G) forces. It mimics an aircraft’s turning motion by spinning, which generates centrifugal forces that act on the pilot. Pilots are taught how to combat the centrifugal forces through the Anti-G Straining Manoeuvre (AGSM), a technique combining lower body muscle tensing and rhythmic chest straining cycles. When AGSM is properly executed, the pilot can maintain consciousness to continue operating the aircraft effectively during flight manoeuvres.
The training is overseen by a medical director and a physiology training officer (PTO). While the PTO teaches the pilot AGSM, the medical director cares for the pilot’s safety, ensuring they are medically fit before and during the training, monitoring their ECG and other vital signs.
Navigating high altitudes
 Dr Robin Low (left) and LTC(DR) Aaron Chua observe the trainee pilots undergoing hypobaric chamber training. The machine simulates the air pressure at high altitudes.
Dr Robin Low (left) and LTC(DR) Aaron Chua observe the trainee pilots undergoing hypobaric chamber training. The machine simulates the air pressure at high altitudes.
Military pilots who fly at high altitudes may also experience hypoxia. The condition could cause pilots to develop a sense of euphoria and experience symptoms such as giddiness, fatigue, hyperventilation, numbness, hot flushes and even tunnel vision. These could impact their judgement during flight and, in cases of severe hypoxia, lead to unconsciousness.
To train pilots to recognise the symptoms of hypoxia and demonstrate its impact on cognitive and physical performance, they are exposed to reduced atmospheric pressure in a hypobaric chamber, which simulates the environment at high altitudes. “The hypobaric chamber training is vital since the time of useful consciousness at high altitudes is extremely short,” shares LTC Koh Tze Kia, F-16 Pilot, RSAF. “The training refreshes my awareness of my personal hypoxia symptoms which can evolve over time. It also sharpens my ability to recognise signs of sudden cabin pressure loss and take timely corrective actions.”
 Dr Robin Low (in background) and LTC(DR) Aaron Chua conduct a debrief for F-16 pilot LTC Koh Tze Kia after his training session in the Human Training Centrifuge.
Dr Robin Low (in background) and LTC(DR) Aaron Chua conduct a debrief for F-16 pilot LTC Koh Tze Kia after his training session in the Human Training Centrifuge.
Recognising hypoxia at an early stage enables the pilot to take quick action — usually donning an oxygen mask if necessary. Fighter pilots who are already wearing masks may need to activate their emergency oxygen supply and descend their aircraft to a safe altitude to prevent severe hypoxia, or land immediately.
Operating this machinery behind the scenes are training executives who execute the training programme workplan, coordinate doctors’ and PTOs’ schedules, and ensure a healthy enrolment rate for each training session. “We play a key role in planning and responding to the RSAF’s training requirements, ensuring the operational readiness of the RSAF, and consequently, Singapore’s defence,” shares Yeo Boon Kiang, Training Executive, SCAC, CGH.
Besides the HTC and hypobaric chamber training, which pilot trainees must undergo in preparation for flight, the ejection seat trainer (EST) is used to teach pilots to adopt the correct posture for safe ejection, while the advanced spatial disorientation trainer (ASDT) trains them to recognise and avoid spatial disorientation. Disorientation can occur when vision is degraded during flight, such as at night or in poor weather conditions. The pilots also undergo advanced night vision training in a realistic and immersive environment.
Ready for take-off
 Mr Jimmy Ng, Assistant Director, SCAC, CGH, observes the occupant in the ASDT. The ASDT teaches pilots that accurate aircraft control and spatial orientation can only be maintained through proper use of flight instruments.
Mr Jimmy Ng, Assistant Director, SCAC, CGH, observes the occupant in the ASDT. The ASDT teaches pilots that accurate aircraft control and spatial orientation can only be maintained through proper use of flight instruments.
While the training is rigorous, pilots emerge fully prepared to handle various operational scenarios. “I have watched trainees grow from cadets to senior commanders; from seeing them grapple with their AGSM as a pilot trainee, to becoming an operational fighter pilot performing flight manoeuvres,” says Mr Yeo.
 A multidisciplinary team comprising an aviation medicine specialist, a physiology training officer and station operators run the EST, which equips pilots with techniques to circumvent injuries that could occur during seat ejection.
A multidisciplinary team comprising an aviation medicine specialist, a physiology training officer and station operators run the EST, which equips pilots with techniques to circumvent injuries that could occur during seat ejection.
As medical technology and aviation continue to advance, CGH remains dedicated to evolving its aviation medicine practice and expanding its understanding of aircrew health. With several collaborations in the pipeline, CGH aims to advance its holistic approach to aircrew healthcare such as fatigue management to address both the physical and cognitive aspects of aviation professionals’ wellbeing. “CGH’s integrated approach to healthcare not only enhances flight safety but also helps preserve our valuable aviation workforce by reducing medical-related attrition, serving to enhance the performance of our aviators, while strengthening the foundation of aviation safety as a whole,” says Dr Robin Low.
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.