Dive into the body’s endocrine system, where glands and hormones play a vital role in regulating everything from blood pressure to glucose levels, and take a look at how Changi General Hospital’s (CGH) multi-disciplinary care helps patients with endocrine conditions.

The endocrine system consists of glands that produce hormones which regulate various bodily functions.
Endocrinology is the medical specialty that deals with hormones, which are chemicals produced by certain organs (endocrine glands) in the body and released into the bloodstream, where they exert effects on various tissues around the body. The body produces more than 50 different hormones, which are instrumental in regulating numerous bodily functions such as mood, temperature, growth and development, metabolic processes including control of blood pressure and glucose, as well as sex and reproduction.
The production of these hormones also changes in response to feedback from the tissues they act on to maintain a healthy body and mind. Conditions that cause hormone levels to become too high or too low can lead to diseases.
Like the crew of a ship, endocrine glands such as the thyroid, parathyroid, pancreas, adrenals and testes/ovaries each have their different but equally important functions, with the pituitary gland as the captain directing their activities to steer the body in a healthy direction.
The endocrinologists at CGH’s Department of Endocrinology provide specialised and holistic care for patients with conditions that involve their endocrine glands. These conditions include diabetes mellitus, hypertension (high blood pressure), obesity and cholesterol disorders, as well as disorders of the bone, thyroid, pituitary, adrenal and reproductive glan

We take a deeper look at two common endocrine conditions and CGH’s one-stop Diabetes, Obesity, Metabolism and Endocrine (DOME) Centre, which caters to patients who require multi-specialty consultation and care.
Hypertension
Blood pressure refers to the force with which your heart pumps blood throughout the body. An individual’s blood pressure can vary from time to time, depending on various factors such as the time of day, the amount of salt intake from food and drinks, physical activity and emotions. As such, it is recommended that blood pressure be taken on more than one occasion and when an individual is in a resting state.


A silent killer
Hypertension, also known as high blood pressure, occurs when the pressure in the blood vessels is too high. Many people with hypertension do not experience any symptoms and it may remain undetected for years. Some people with hypertension may experience increased headaches, shortness of breath or nosebleeds. However, these symptoms are not specific to hypertension as they may also be present in other diseases. The only certain way to detect hypertension is through measuring the blood pressure. If left untreated, or not properly managed, hypertension can cause further health complications including heart attack, heart failure, stroke and kidney failure.

Diagnosing endocrine hypertension
Most patients with hypertension have essential (unexplained) hypertension and have to be treated with lifelong medications. However, 5-10% of all patients with hypertension may have underlying conditions, which may lead to the improvement, or cure, of hypertension following treatment. In particular, the adrenal glands — which are part of the body’s endocrine system — may produce too much of a hormone, like aldosterone, which can lead to hypertension occurrence.
Patients with too much aldosterone often develop hypertension and low potassium levels (hypokalemia). This is an important condition to treat, as patients with high aldosterone levels often have difficult-to-control hypertension, and are at greater risk of heart and kidney disease. In addition, this is a curable cause of hypertension, and early treatment makes it more likely for patients to be cured.

Managing the pressure
“Hypertensive patients should have their aldosterone and renin levels checked at least once, especially if they have low potassium levels,” says Clin Asst Prof Troy Puar, Senior Consultant, Department of Endocrinology, CGH.
“While hereditary risk factors are non-modifiable, there are other actions that can lower the risk of hypertension.”

Steps can be taken to lower the risk of hypertension.
For example, reduce or stop smoking, limit alcohol intake, eat a healthier and balanced diet and exercise regularly to achieve a healthier Body Mass Index (BMI) — exercise can also help to lower the blood pressure and manage stress. “If you have other health conditions, take the medications consistently and go for reviews as needed. If you are constantly stressed, make time to rest and try to have adequate sleep. Additional treatments may be needed to manage the hypertension,” says Clin Asst Prof Puar.
Managing hypertension at CGH
The CGH Adrenal Hypertension Centre was established in 2023 to offer comprehensive evaluations for patients with hypertension that is caused by excessive adrenal hormones. These evaluations include blood and urine tests for excess hormones.
The Shimadzu-CGH Clinomics Centre (SC3) was launched in 2021, and currently runs hormone tests using mass spectrometry, eliminating the need to run the tests overseas.
At these centres, CGH’s multi-disciplinary team, involving endocrinologists, radiologists, laboratory medicine specialists, histopathologists and surgeons, work together to diagnose and treat patients with various adrenal conditions, such as primary aldosteronism, pheochromocytoma and Cushing’s.
![]()
Adrenal Hypertension Patient Support Group
CGH recently started a patient advocacy group for patients with hypertension — the first meeting will be held in May 2024 in conjunction with World Hypertension Month
Diabetes

The pancreas produces insulin, which regulates glucose levels in the body.
Diabetes Mellitus, commonly known as diabetes, is a chronic disease where the sugar levels in the blood are abnormally high.
Most of the food we eat is converted into glucose upon digestion, which enters the bloodstream. Insulin then moves the glucose from the bloodstream into the body cells for use as energy or storage. Insulin is a hormone produced by the pancreas that regulates the glucose level in the blood.
If the pancreas does not produce enough insulin, or if the body is unable to effectively use the insulin, glucose is unable to enter the cells and accumulates in the bloodstream, resulting in diabetes.
Honeyed hints
While mild diabetes is often without symptoms, one may experience increased thirst, frequent urination, intermittent blurred vision, slow-healing sores or frequent infections or even weight loss when the sugar levels in the bloodstream are significantly increased. If not properly managed, diabetes can lead to complications such as blindness, chronic kidney disease, amputations, heart attack or stroke.
These symptoms might indicate that further tests are required to determine the diagnosis. Blood glucose tests include a fasting blood glucose level test, a random blood glucose level test and an oral glucose tolerance test.

Type 1 diabetes
Type 1 diabetes is an autoimmune condition where the body’s immune system attacks and destroys the beta cells (the cells that make insulin) of the pancreas. The damaged pancreas is then unable to produce insulin, and the body cells are unable to absorb glucose from the bloodstream. Persons with this condition will require lifelong insulin injections. Type 1 diabetes affects 5% of all people with diabetes.
Type 2 diabetes
In Type 2 diabetes, the body’s cells require more insulin than usual to absorb glucose from the bloodstream, due to resistance that has developed towards insulin. Being unable to produce enough insulin to cope with these increased needs, glucose levels rise.
Common causes of Type 2 diabetes:
- Overweight or obesity
- Sedentary lifestyle
- Family history of Type 2 diabetes
- High blood pressure (above 140/90mmHg)
- Abnormal cholesterol levels
- Gestational diabetes, or previously delivering a baby weighing more than 4kg

Lowering the risk
“Prevention is better than cure. The key to lowering the risk of getting Type 2 diabetes is making lifestyle changes for the better,” says Dr Zeng Wanling, Consultant, Department of Endocrinology, CGH.
Some tips include:
Maintain a healthy diet with an emphasis on vegetables, fruits, nuts, fish and whole grains and avoid sugar-sweetened beverages and snacks
- Have 150 to 300 minutes of moderate-intensity physical activity per week
- Maintain a healthy BMI
- Stop smoking
- Limit alcohol intake
Managing diabetes
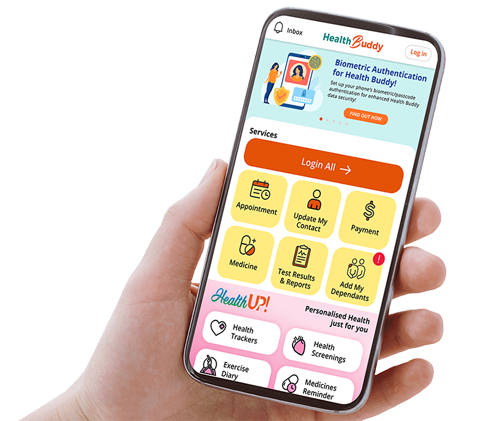
As a smart hospital, CGH integrates technology into the care for patients. Integrated technologies such as the continuous glucose monitoring (CGM) device and insulin pumps help to improve glucose control, patients’ quality of life, and facilitate the self-management of diabetes.
The CGM device monitors blood glucose levels by using a sensor inserted under the skin to measure the interstitial glucose level. It allows the patients to monitor their glucose levels throughout the day without the need for finger pricks. “Patients can share their glucose data with our CGH care team through a secure cloud-based platform to enable us to make adjustments to their treatment regimen,” explains Dr Zeng.
The insulin pump is a battery-operated device inserted into the subcutaneous layer of the abdomen to deliver continuous insulin (basal insulin) and rapid acting insulin (bolus insulin) into the bloodstream. The hybrid closed loop (HCL) pump is an advanced insulin pump with the ability to deliver variable amounts of basal insulin and bolus insulin automatically, based on the glucose readings obtained by the CGM device. This enables patients to receive the customised amount of insulin required.

Savouring every Moment

Mr Khor believes that proper
care of diabetes enables him
to still do the things he enjoys.
Even though Mr Gilbert Khor has Type 1 diabetes, he continues to live life to the fullest with his family.
Over 10 years ago, Mr Khor started experiencing a drastic drop in weight and frequently blacked out when climbing the stairs. After being referred to CGH, it was found that Mr Khor had diabetic ketoacidosis (DKA), a serious complication of diabetes common among people with Type 1 diabetes — which Mr Khor was then diagnosed with.
Over the years, Mr Khor transited to an insulin pen, and in 2022, he started on the CGM device and insulin pump. “I decided to sign up for the CGM device and it has provided great convenience when holidaying or when I go for meals, as I can adjust the insulin doses to be administered on the go,” says Mr Khor. “Dr Zeng and CGH Senior Nurse Manager Authilakshmy D/O N M have been great companions on my diabetic journey. Dr Zeng continually seeks ways to help with the management and betterment of my health by understanding more about what I do and eat, providing advice based on them and getting me additional support from the other specialists. The nursing team has also been a great support, ensuring that I am well taken care of and in the best of health.”
While diabetes prevention is important, Mr Khor, now 39, wants to also encourage those with diabetes not to fear the disease but to manage diabetes with proper care, so that it does not impact the quality of life significantly.
CGH DOME Centre
The CGH Diabetes, Obesity, Metabolic and Endocrine (DOME) Centre manages and treats patients with diabetes, hypertension, obesity and other endocrine disorders with its multi-specialty practice. For instance, patients with diabetes are likely to also have weight management issues, hypertension and related conditions. Instead of visiting several clinics for treatment, patients can see two or more of CGH’s multi-disciplinary care team at the DOME Centre to better manage their chronic diseases.
Hormonal harmony with endocrinologists
“The entire care team at the CGH DOME Centre plays an important role in caring for our patients. The endocrinologists help patients with diabetes manage and maintain their blood glucose levels within a target range, monitor the development of complications and provide self-management education and support to empower patients and their families to allow them to care for themselves,” says Dr Zeng.

Together with the multi-disciplinary team, the endocrinologists enhance the care outcomes of patients.
CGH endocrinologists also oversee and coordinate the overall care of the patients, working with different members of the multi-disciplinary care team to enhance the care and outcomes of the patients. For example, if more intensive monitoring of the blood sugar and adjustment of insulin regimen is required, the endocrinologist will refer the patient to the diabetes nurse educator (DNE). If the endocrinologist identifies diet as a major factor that affects a patient’s management of diabetes, they will refer the patient to the dietitian. “We also support our patients through the various stages in their life journey as we have a long-term patient and doctor relationship,” says Dr Zeng.
Nursing care
CGH nurses at the DOME Centre not only provide routine care, but also support patients with hypertension through monitoring tests such as salt loading (determining how the body handles salt by producing a hormone that regulates blood pressure) and Synacthen tests (assessment of the adrenal glands’ functions). For patients with diabetes, the nurses conduct diabetes complication tests such as retinal photography and foot screenings.
“Patient education is a key role of the DNEs at the DOME Centre,” says CGH Senior Nurse Manager Authilakshmy D/O N M. “It tends to be for newly-diagnosed patients, or those initiated on a new diabetes therapy.” DNEs play a pivotal role in reducing hospital readmission rates and preventing delayed discharges. Utilising technology, the nurses also monitor patients’ blood glucose levels and make insulin adjustments through telemonitoring.
The DNEs also work closely with the dietitians, conducting joint counselling sessions for patients on insulin therapy. During these sessions, patients are taught carbohydrate counting and how to calculate their insulin doses for their meals.
For patients in the community, the CGH nurses conduct patient empowerment workshops to educate them on how to monitor their glucose levels and skills for diabetes management.
 Nurses conduct diabetic retinal photography screenings to detect diabetes complications.
Nurses conduct diabetic retinal photography screenings to detect diabetes complications.
Nourishing wellness
“During the consultations, dietitians conduct nutrition assessment based on information about patients’ weight, biochemical, clinical, dietary, physical activity, and social factors,” says Ms Fionn Chua, Senior Dietitian, CGH. “To support patients in making positive changes, we provide them with the required knowledge, and guide them to make informed choices about their dietary habits to better manage their medical conditions.”

CGH’s nurses and dietitians conduct multi-disciplinary team clinic consultations for patients with diabetes at the Joint Dietitian and DNE (JDD) sessions.
Many patients have multiple comorbidities and require individualised dietary counselling to help them achieve their health goals. For patients with hypertension who also struggle with weight management, CGH dietitians explain the theory behind how diet can help with weight loss and blood pressure control, and provide practical advice on how to achieve a lower sodium or lower calorie intake in their diet.
For patients newly diagnosed with diabetes, the dietitians provide comprehensive explanations on the link between diet and disease. “For example, patients need to know about the sources of carbohydrates and their impact on the blood sugar level, so that they can take the right steps in changing their diets,” says Ms Chua.

Dietitians at the CGH DOME Centre provide patients with dietary counselling based on their conditions.
CGH dietitians also aid other groups of patients at the Centre, including patients undergoing bariatric surgery, renal patients — such as those on peritoneal dialysis — and patients with lipid disorders.
Best foot forward
At the CGH DOME Centre, CGH podiatrists primarily provide care for patients with diabetes, and educate them in taking responsibility for their foot health. Foot wounds are common complications that arise from nerve damage, foot deformities, poor circulation, external trauma such as poorly-fitted footwear, or amputations. Podiatrists remove dead or unhealthy tissue from a patient’s wound, and apply appropriate strategies to redistribute pressure on the foot, preventing infections and facilitating wound healing.

CGH podiatrists ensure optimal foot health for diabetic patients, an important aspect of maintaining their overall health.
Many diabetic patients have skin and nail abnormalities such as ingrown nails, fungal nails, calluses and corns. When patients and caregivers are unable to do so appropriately, podiatrists help with specialised trimming and removal. “In a diabetic patient with inadequate blood supply to the lower limb, ingrown nails can result in a non-healing wound, possibly gangrene and toe amputation,” says Ms Kuah Bao Peng, Principal Podiatrist, CGH.
Offloading (reducing and redistributing pressure to areas of the foot) is another critical aspect in preventing wound recurrence. “We prescribe customised insoles for patients or refer them to our orthotist for footwear modifications based on our knowledge of our patients and the insole’s material properties,” says Ms Kuah.
Driving precision in hypertension diagnosis
Changi General Hospital (CGH) redefines the diagnosis of salt-sensitive and curable forms of hypertension with technology.

Ms Tan Yi Ting, Research Associate, CGH, carries out research and assists to process blood samples sent for testing at the SC3.
The Shimadzu-CGH Clinomics Centre (SC3) clinical service leverages liquid chromatography and artificial intelligence (AI)-assisted mass spectrometry, allowing for the precise measurement of two hormones — aldosterone and renin. This advancement is crucial in differentiating and diagnosing salt-sensitive hypertension and primary aldosteronism, a lesser-known yet curable form of hypertension.
Reaping the fruits of research for patient-centric healthcare outcomes
In Singapore, about 5% of all patients with hypertension have the curable form of primary aldosteronism hypertension, yet many are not screened and treated. For these patients, the underlying cause of their high blood pressure is an abnormal growth in one or both of their adrenal glands, which are responsible for producing hormones that help to regulate blood pressure. Through a keyhole surgery to remove the growth in the adrenal gland, a patient with primary aldosteronism may significantly improve or be totally cured of their hypertension.
Prior to the establishment of the SC3, the testing of hypertensive patients’ blood specimens had to be sent to overseas laboratories, where results often took several weeks. Now, specimens can be processed locally, allowing for shorter turnaround times of three to five days. This enables more patients to be successfully tested, diagnosed by doctors, and treated with precise care. To date, CGH has conducted over 1,000 clinical tests in patients with hypertension.
The shift to local testing at the SC3 has also made a noticeable difference in patient care. Quicker test results lead to a more enhanced patient journey from testing to treatment, thus reducing stress and uncertainty for patients who have lived with hypertension — often uncontrolled — for many years.
One such patient is Mr Khoo Keow Pin, 66, who struggled with the condition for more than 15 years, having been unaware that he had primary aldosteronism and the fact that it is curable. Following testing at the SC3 and his diagnosis in June 2023, Mr Khoo underwent an adrenalectomy surgery at CGH in September 2023 to remove his affected adrenal gland. Just two weeks after his surgery, Mr Khoo’s condition improved significantly. Today, he requires less medications and his blood pressure — which is now at a normal level — has stabilised for the first time in several years.

Mr Khoo undergoing the salt-loading drip test as part of testing for primary aldosteronism.
“I believe in the importance of testing, especially for long-term hypertension patients like myself,” says Mr Khoo. “With the quick and detailed investigations done at SC3, the doctors were able to arrive at the accurate diagnosis of my type of hypertension — primary aldosteronism — enabling me to seek treatment at CGH and improve my condition.”
Technology for tomorrow
The use of liquid chromatography, mass spectrometry and AI marks a significant shift from traditional diagnostic methods, and presents clinicians with a more nuanced understanding of the two types of hypertension. Dr Daryl Hee, Assistant Director, CGH, who oversees the SC3, explains: “The mass spectrometry technology used at the SC3 is equipped with a unique algorithm incorporating AI assistance. With machine-learning capabilities, the AI employed at SC3 can process test data at a high skill level. This allows us to pick up the correct chromatography peaks and measure plasma aldosterone and renin activity even when present at very low concentrations.”

The AI-assisted algorithm at the SC3 can process data at heightened accuracy.
The two tests have been rigorously validated based on CLSI (Clinical & Laboratory Standards Institute) guidelines.
“Being part of this research in the early stages to the translation to a full-fledged clinical service in February 2023 — and eventually seeing such improved patient outcomes from the tests that we have developed collectively with clinicians and laboratory medicine colleagues — is indeed a rewarding and fulfilling experience,” shares Ms Tan Yi Ting, Research Associate, CGH, who was involved in developing the tests at SC3.

Serving as a regional reference centre, the SC3 is also developing unique mass spectrometry solutions, including catering to various clinical diagnostics and applications for other chronic conditions, to more countries in the Asia Pacific region.