Making no bones about it
- Issue 3
- Making sense of musculoskeletal conditions
- Caring for your body
- Making no bones about it
- Journeying with patients through the times
- Celebrating mothers (and daughters) in healthcare
- Pin-pointing remedies
- Inspiring nurses to innovate
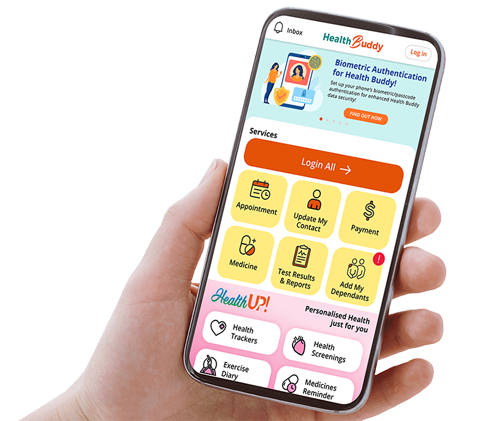
- What's up, Bot?
- A wellness ecosystem for the young
- Bettering your bladder and bowel care
- Cheers to kindness and patience
- Breathtaking facts about asthma
With our musculoskeletal system consisting of muscles, bones, joints, ligaments and tendons that make up our entire body, it is no coincidence that Changi General Hospital’s (CGH) orthopaedic body of care consists of a multi-disciplinary team to provide a full spectrum of care.

Associate Consultant,
Orthopaedic Surgery
A medical team helmed by orthopaedic surgeons and consisting of orthogeriatricians and anaesthetists works together closely to provide expedient specialised care for patients. Research has shown that safe and early surgery improves recovery outcomes, and CGH’s dedicated team of experienced surgeons is equipped to handle these injuries and conditions.
“I am an orthopaedic surgeon in the trauma team, with interests in hip and knee surgeries. The orthopaedic team sees about 500 hip fractures a year at CGH in our increasingly elderly population. Resources are appropriately allocated for the timely management of patients with hip fractures, allowing us to perform the surgeries expediently to help our patients on their way to regaining their functional independence,” he says.
“Patients are then monitored post-surgery by the orthopaedic team and therapy is commenced early with the support of our allied health colleagues to get patients back on their feet as soon as possible!”

Mohamad Mascuri,
Advanced Practice
Nurse / Nurse Clinician
The multi-faceted role of an orthopaedic advanced practice nurse (APN) entails providing care for patients with musculoskeletal conditions including broken bones, arthritis, osteoporosis, joint replacement and other injuries and diseases. One of the treatments that the nursing team administers is the setting up of tractions (a system of weights, pulleys and ropes to realign broken bones) and backslabs (a slab of plaster on one side of the limb) at patients’ injury sites to immobilise their broken bones while life-threatening conditions are being attended to.
For post-operative patients, the nursing team works closely with the surgeons in wound management and ensures optimal pain control. “As nurses, we work alongside physiotherapists and occupational therapists to promote early mobilisation,” she says. “We also consult dietitians to discuss nutrition care plans, and with pharmacists on the appropriate dispensing and dosage of medicines.”


Physiotherapist
Physiotherapy in an orthopaedic setting can be described as “giving life to what is injured, broken or repaired in our body”. As a physiotherapist, Elvin aims to improve joint range and muscle strength, and provide pain relief to optimise the function of individuals. The physiotherapy team assesses, manages and treats the impairments of patients with orthopaedic injuries so that they can reach their optimal function within the shortest period of time. “We are involved in the care of our patient’s rehabilitation journey during conservative management (treatment without undergoing any surgical procedure), before and after their operation,” he says. “Patients and their caregivers are educated on the suitable exercises and strategies to facilitate healing and the use of walking aids, if applicable, that may be required at different stages of their rehabilitation journey.” Physiotherapists also communicate with other care team members on any limiting factors — such as pain, numbness, reduced social support etc. — to help patients optimise their recovery.


Radiographer
Radiographers act as the eyes of doctors to provide the first line of diagnosis for patients after their treatments have been administered. “We perform radiographic examinations to look at patients’ bones and muscles pertaining to their injuries,” she explains. “X-rays are usually the fundamental tool for diagnosing an injury before patients see the doctor. In addition, patients may require examinations like Computed Tomography (CT), ultrasound and Magnetic Resonance Imaging (MRI) scans to plan for their surgeries.”
“With our help in providing professional and quality radiographic examinations, our patients’ prognosis can be improved with the best interventions and treatments planned in a timely manner,” she says.


Occupational Therapist
An occupational therapist’s role in the rehabilitation team is to help patients work towards independence in daily activities. These include activities ranging from basic self-care such as using the toilet, taking a shower and putting on clothes to resuming valued hobbies and routines such as returning to work or school.
Noelle works with each patient to explore the possibility of continuing to do things in the same way as before their injury and practises the task with them so that they can regain their independence. She also assesses the home environments of patients, and suggests modifications to increase accessibility and safety within the house.
“I may teach different compensatory ways of doing the same task,” she explains. “For example, I may explore alternate methods of wearing a shirt for a patient with a rotator cuff injury who is unable to raise his/her arm sufficiently when threading the sleeves, or wheelchairs suitable for patients who have difficulty walking.”

Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.