Delve into Changi General Hospital (CGH)’s latest advances in geriatric medicine and care, with strategies and solutions designed to enhance the health and well-being of seniors.

A multi-disciplinary team assessing a senior at the Geriatric Day Hospital.
With a rapidly ageing population, Singapore is faced with an increase in the unique healthcare needs of older adults. Geriatric medicine focuses on the healthcare needs of the seniors, who often are frail and tend to have multiple medical issues, and face physical, functional and social challenges. Addressing these challenges requires a multidimensional approach and multiple interventions to achieve good clinical outcomes.
Geriatric medicine at CGH began in 1998. It expanded to over 190 beds across five acute geriatric wards and a stroke rehabilitation ward, as well as a subacute ward when the Integrated Building opened in 2015. The Integrated Building provides a seamless healing environment for patients across hospital and rehabilitation settings, including the eventual transition of patients back to their homes. The CGH Department of Geriatric Medicine collaborates with various specialties such as orthopaedics (orthogeriatric service), general surgery (geriatric surgical service), the Emergency Department, the Dementia and Delirium Outreach Team and the acute medical unit to deliver care to seniors.

In 2005, CGH set up the Community Geriatrics Service with a focus on establishing systems of comprehensive care for older adults beyond the hospital setting.
“CGH’s comprehensive range of integrated geriatric services will continue to grow and innovate to meet the evolving needs of seniors, and their family members or caregivers. We are focused on delivering holistic person-centred geriatric care across the healthcare spectrum, from the emergency department and acute inpatient wards across all disciplines, to intermediate and long-term care institutions as well as the wider community,” says Dr Goh Kiat Sern, Head, Department of Geriatric Medicine, CGH.
The Geriatric Medicine Centre
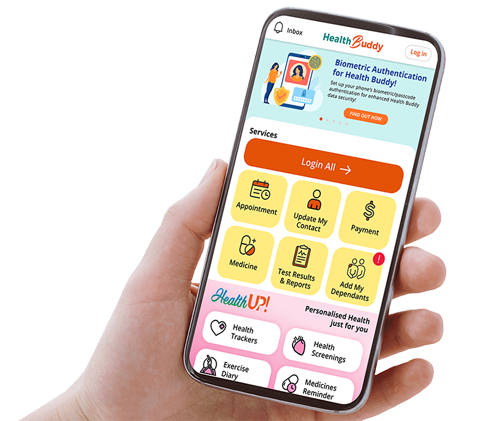
The CGH Geriatric Medicine Centre (GMC) serves as a one-stop facility tailored to seniors experiencing complex medical conditions. Located on level 2 of the Integrated Building, the GMC comprises various specialty clinics for outpatient appointments and houses the Geriatric Day Hospital. The GMC manages approximately 23,000 visits a year.
These clinics are designed specifically to manage senior patients with multiple medical and geriatric conditions. Every new patient referred receives a comprehensive assessment to determine their care needs. These needs are then integrated into a personalised care plan. When necessary, patients may also be referred to other medical disciplines, dietetic and rehabilitative services, or even external agencies, to assist in the management of care.

A physiotherapist conducting a session at the Geriatric Day Hospital.
“Besides geriatric care, specialty clinics at GMC are run by psychogeriatricians, who are psychiatrists who tend to senior patients to address their psychiatric and behavioural issues,” says Dr Low Shou Lin, Senior Consultant, Department of Geriatric Medicine, CGH. “This is complemented by psychotherapy conducted by psychologists and supported by occupational therapists. Dietetic clinics provide dietary and nutritional guidance for senior patients with poor oral intake and weight loss.”
Additionally, trained nurses offer patient education on managing conditions like dementia and falls — which enhances patient and caregiver confidence — and following treatment plans.
CGH runs the following clinics within the Geriatric Medicine Centre:
- Falls Clinics assess and manage patients with falls.
- Memory Clinics are jointly run by geriatricians and psychogeriatricians. They provide specialised care for individuals experiencing memory impairments.
- The Continence Clinic assesses and treats senior patients with urinary incontinence, and provides education on bladder retraining and the use of continence aids.
- The Frail To Fit Clinic is specifically targeted at assessing and managing vulnerable frail seniors in a holistic manner.
- The Stroke Clinic provides post-stroke care to older patients. It addresses and optimises vascular risk factors, which include improving blood pressure, getting lipids to target levels, controlling diabetes, and ensuring that the patients are on a healthy diet that is modified to their needs.
- The Parkinson’s Disease Clinic delivers proactive multidisciplinary care to seniors with Parkinson’s disease, in partnership with neurologists from the National Neuroscience Institute and various allied health practitioners.
- The Wound Clinic is a clinic led by Advanced Practice Nurses and supported by geriatricians to manage senior patients with complex wounds.
Geriatric Day Hospital
Singapore’s only Geriatric Day Hospital (GDH) at CGH is helmed by an experienced team comprising geriatric-trained doctors, nurses, physiotherapists, occupational therapists and a medical social worker. The GDH allows for easy and quick access to assessments, investigations, medical treatments and rehabilitation for frail patients with a wide range of medical conditions. It offers a short-term programme that targets medical stabilisation and functional improvement for outpatient patients with complex medical needs — such as Parkinson’s disease, frequent falls and strokes — to promote independence at home and reduce caregiver burden.
Before enrolment, a geriatrician assesses each patient for suitability. Once enrolled, patients undergo weekly half-day sessions that include physiotherapy and occupational therapy.

A CGH doctor having consultation with a senior at the Geriatric Day Hospital.
After a maximum of 12 sessions, patients make the transition to appropriate community-based services.
Caregivers play an integral part in the lives of older adults by providing care and assistance. Caring for patients with dementia can be stressful. To support patients with dementia and their caregivers, CGH launched the GDH Engage Programme in March 2021. This six-week programme combines cognitive stimulation therapy for patients and educational sessions on dementia progression, behaviour management strategies and caregiving resources, delivered by a multi-disciplinary team.
Community Geriatrics
The CGH Community Geriatrics Service aims to address the unique healthcare needs of older adults living in the community. This includes identifying and managing common geriatric conditions, reviewing chronic conditions, preventing disability, improving quality of life and promoting healthy ageing.

A patient learning to use exercise
equipment under the guidance
of the physiotherapist and doctor
at the Geriatric Day Hospital.
“Through various meaningful programmes, our community geriatrics team supports older adults in the community, empowering them to live well, identify age-related health issues promptly, prevent or minimise disability, and maintain dignity as they age,” says Dr Samuel Ee, Associate Consultant, Department of Geriatric Medicine, CGH. “The multi-disciplinary team collaborates with community partners for sustainable and holistic care to meet their clinical, physical, mental, emotional and social needs.”
A comprehensive geriatric assessment is usually the first step to help identify the relevant needs of an older adult. Subsequently, individuals may benefit from interventions such as medication management, falls assessment and prevention programmes, advance care planning and — where appropriate — palliative care.
In addition, caregiver education, support and the coordination of care with other healthcare providers may be necessary as well to help them minimise and cope with burnout. These services aim to help older adults maintain independence, improve well-being, and enhance quality of life as they age in their own homes or community settings.
In caring for the community, CGH community geriatricians work in various settings including nursing homes and community hospitals, and also support community-based multi-disciplinary teams (such as community nurses and care coordinators). More complex patients require greater interdisciplinary collaborations with physiotherapists, occupational therapists, care managers and social workers from various social agencies, as needed.
Community geriatricians also support the transitional care service in CGH known as Hospital to Home, whereby older adults with complex care needs are managed together with community nurses and allied health professionals in the home setting.
Community partners also include primary care physicians as part of the Geriatric Service Hub (GSH) model, where seniors are actively screened for age-related health issues, some of which require multi-disciplinary care. This is in turn supported by CGH community geriatricians, CGH community nurses and well-being coordinators.
CGH also works with nursing homes in Eastern Singapore as part of the Enhancing Advance Care Planning, Geriatric Care and End-of-Life Care in the Eastern Region (EAGLEcare) programme. “EAGLEcare improves the delivery of geriatric and end-of-life care to nursing home residents, and empowers nursing homes to attend to residents who may be heading towards their last year of life so that concerns and options of care can be pro-actively discussed with family members,” says Dr Christopher Lien, Senior Consultant, Department of Geriatric Medicine, CGH. “Towards the terminal stages of life, the team supports the care in nursing homes, helping residents to remain comfortable, meet their care preferences, and minimise avoidable hospital admissions.”
The Multi-faceted Role of Nurses in Geriatric Care at CGH

Nurses encourage patients to sit
out of bed and engage with social
robots for physical activities during
their hospital stay.
Nurses at CGH play a crucial and multi-faceted role in the care of senior patients, providing comprehensive services that meet the unique physical, emotional and social needs of this population. They assess and manage chronic conditions such as diabetes and dementia, and develop individualised care plans to enhance functional independence, mobility and overall quality of life.
“As a Nurses Improving Care for Healthsystem Elders (NICHE) member hospital, we are dedicated to driving geriatric nursing care to its apex, delivering compassionate, person-centered care that empowers seniors to thrive,” says Adjunct Associate Professor Png Gek Kheng, Chief Nurse, CGH.
One practical aspect of care involves promoting mobility among senior patients, which is crucial for maintaining physical health and independence during hospitalisation. A nurse-driven mobility protocol was put in place to promote mobility of the senior patients and to prevent functional decline. Activities such as assisting patients to sit out for meals and facilitating walking around the ward significantly enhances mobility and fosters social interactions, contributing to a robust community atmosphere and overall well-being.
Moreover, CGH nurses provide essential emotional support and counselling to both patients and their families, aiding them in navigating the challenges associated with ageing and chronic illnesses. This support is particularly vital for families of patients progressing through stages of dementia, offering guidance through the difficulties they face.
“Besides providing holistic and person-centred care, our nurses advocate for the rights and dignity of patients,” adds Dr Li Fuyin, Senior Nurse Clinician (Advanced Practice Nurse), CGH.
Transforming Geriatric Nursing Care

A CGH nurse shares resources with a
patient through a tablet.
CGH has adopted the Fulmer SPICES1 model, which provides a comprehensive framework for geriatric nursing care that caters to the assessment of unique needs of senior patients who are hospitalised.
Fulmer SPICES stands for six key areas:
- Sleep disorders
- Problems with eating or feeding
- Incontinence
- Confusion
- Evidence of falls
- Skin issues
A series of evidence-based nursing protocols were implemented by CGH nurses for holistic and effective management of senior patients:
- Postural hypotension protocol to manage the condition and fall risks
- Mobility protocol
- Delirium care bundle to promote cognitive health in senior patients with dementia or delirium
- Pressure injury care bundle to promote skin health
- Sleep hygiene protocols for non-pharmacological management of sleep disturbance
Additionally, the Nurse-led Integrated Care for Elders (NICE) training programme has been implemented to equip non-geriatric ward nurses with the knowledge necessary to champion and manage geriatric care effectively, thus promoting best practices in clinical settings to deliver care that matters.
Fulmer, T. (2007). How to Try This: Fulmer SPICES. AJN, American Journal of Nursing, 107 (10), 40-48. doi: 10.1097/01.NAJ.0000292197.76076.e1.
Allies in restoring health and well-being
Changi General Hospital (CGH) allied health professionals restore, maintain and enhance the physical, cognitive and social functions for patients’ overall health and well-being from hospital to home.

Speech therapists help patients understand and interact with their loved ones.
Restoring strength, balance and mobility
CGH physiotherapists focus on helping senior patients regain strength, balance and mobility to maintain their function as long as possible.
“We emphasise on the importance of falls prevention and promote active lifestyles. Common issues faced by seniors include balance, which leads to falls and injuries, often necessitating surgery or immobilisation.
We harness advanced rehabilitation equipment and assistive robotic devices to facilitate movement rehabilitation. Our comprehensive evaluations of patients consider not just physical but also psychosocial factors, ensuring personalised care plans that are developed by the CGH multi-disciplinary care team. These plans may include exercise prescriptions and caregiver training to support patient needs in a comprehensive manner.
As part of preventive care under Healthier SG, our therapists work on optimising seniors’ functional independence, and equipping them with knowledge to maintain fitness and well-being when they are back at home and in the community.”
Lai Ka Ying, Principal Physiotherapist, CGH

Occupational therapists help patients
improve their daily function during
their hospital stay.
Supporting daily activities through person-centred care
Occupational therapists at CGH assess and assist senior patients with cognitive impairments and daily activities, providing person-centred care.
“We view each patient as a unique individual, and consider their life experiences and personal values in our support strategies.
Patients with dementia often exhibit challenging behaviours, which we interpret as expressions of unmet needs. Our care includes educating families to understand and manage these behaviours effectively, enhancing the well-being of patients and easing caregiver burden.
Our goals are set collaboratively with patients and caregivers, and we aim to enable patients to live meaningfully in the community despite the challenges they may face. With Singapore’s ageing population, our role is crucial in helping seniors maintain dignity and in reducing the caregiving load on families.”
Lydia Thio, Occupational Therapist, CGH
Empowering communication and swallowing
Speech therapists assist senior patients affected by conditions like dementia, stroke, and Parkinson’s disease, which can impair communication and swallowing.
“Our goal is to help these patients interact meaningfully with loved ones and ensure they can safely enjoy their meals. We manage patients across settings, from inpatient wards to outpatient clinics, and in the community, such as at their homes or nursing homes.
Many senior patients face difficulties due to weak hands or swallowing disorders, necessitating innovative devices like the CGH Drink-Ezy cup, which allows more independent drinking. We also use iPad applications to support communication therapy, helping stroke patients with word-finding difficulties and enhancing speech clarity and loudness.
Our approach is tailored, as we recognise the varied therapy needs of senior patients in light of the increasing challenges faced by those with Parkinson’s disease or dementia. By closely working with patients and their caregivers, we design specific interventions that address their unique situations.”
Lee Yan Qing, Principal Speech Therapist, CGH
Optimising seniors' health through nutrition
By Ms Chong Hui Hsien, Principal Dietitian, Department of Dietetics, CGH
As individuals age, their nutritional needs change, making optimal health maintenance increasingly important.

Factors like less-active lifestyles, poor digestion, reduced sensory perception, dental issues and swallowing difficulties can impact the ability of seniors to meet their requirements of calories, protein, fibre, vitamins and minerals. Changi General Hospital (CGH) dietitians specialising in geriatric nutrition play an important role in supporting seniors in achieving balanced nutrition and overall well-being.
Key nutritional challenges managed by CGH dietitians include:
- Malnutrition: It is common for seniors to lose weight and appetite as they age, which is not ideal. Carrying a little extra weight can be beneficial during illnesses or when appetite is poor. Dietitians work to prevent malnutrition through a personalised “food first approach” to nutrition and hydration, recommending food fortification and supplements as needed to enhance nutrient intake and prevent frailty.
- Chronic Diseases: Dietitians provide advice to manage diseases like diabetes, hypertension and heart disease, helping stabilise these conditions and prevent complications.
- Swallowing and Dental Issues: Collaborating with speech therapists, dietitians help manage suitable diets for those with swallowing difficulties, ensuring safety and minimising choking risks.
- Dehydration and Constipation: Advice on a fibre-rich diet and adequate fluid intake is given to prevent constipation and promote regular bowel movements. Staying hydrated is emphasised as seniors are prone to dehydration due to thirst perception.
- Protein Intake: Adequate protein is essential for maintaining strength and independence. Dietitians advise on incorporating suitable protein into diets — especially for those with poor dentition or swallowing difficulties — and may recommend oral nutritional supplements.
- Osteoporosis and Fractures: Dietitians provide guidance on adequate calcium and vitamin D intake to prevent osteoporosis and fractures.
CGH dietitians are essential partners in the multi-disciplinary care team, ensuring that seniors receive a nutrient-dense diet to maintain physical health, mental alertness and a fulfilling life. They effectively communicate nutrition concerns and integrate dietary plans with overall care strategies in collaboration with other health professionals.
A Healthy Snack Recipe for Seniors
Soymilk Custard

Practically effortless to make, this delicious, lactose-free custard can be prepared under 30 minutes. Substitute the fruit toppings with other fruits as desired.
Ingredients (Serves 2)
- Egg whites 100ml
- Soymilk 200ml
Toppings
- Peach slices 2-3 slices, finely diced
- Cherry 2, finely diced
- White dragon fruit ¼, peeled and finely diced
- Almond flakes a handful, roasted
Method
- In a mixing bowl, combine egg whites and soymilk. Mix well and strain through a fine wire sieve.
- Pour mixture into prepared heat-proof serving glasses and steam over high heat for 8 minutes, or until custard is set.
- Garnish with toppings and serve hot.
*Recipe adapted from a CGH cookbook for diabetics.
Benefitting older adults through research and innovation
As we grow older, our immune systems may not work as well and there is an increased prevalence of chronic diseases.

A CGH nurse conducts group therapy at the Geriatric Day Hospital with its good helper — a social robot.
Reversing frailty through frailty research
One of the key health concerns for older adults is frailty, which involves a gradual decline in multiple organ systems, leading to increased risks of falls, delirium, disability, hospitalisation and mortality. Recognising the importance of assessing frailty and introducing frailty interventions, Changi General Hospital (CGH) conducted research on the assessment of the frailty status of older adults, who were hospitalised for a heart attack, through a comprehensive risk score.
CGH’s study revealed that patients at high risk of frailty — as identified by the Hospital Frailty Risk Score (HFRS) — had significantly longer hospital stays, and higher mortality rates compared to those at low risk of frailty. These findings highlight the efficacy of the HFRS in stratifying patients and guiding clinical decision-making to improve outcomes.
“Frailty is prevalent among older adults and is associated with higher healthcare utilisation, including emergency admissions and extended hospital stays. More importantly, frailty can be slowed or even reversed through timely interventions that optimise functional ability, promote activity participation and enhance the quality of life,” says Dr Barbara Helen Rosario, Senior Consultant, Department of Geriatric Medicine, CGH. “Through the use of the HFRS and comprehensive frailty management programmes at CGH, we strive to enhance the health and well-being of older adults in the hospital and in the community.”
Transforming geriatric nursing through innovative technologies
The introduction of innovative technologies has revolutionised nursing care for older adults at CGH. A collaboration by the multi-disciplinary care team with the Centre for Healthcare Assistive and Robotics Technology (CHART) at CGH, social robots were designed and programmed with clinical inputs from nurses, physiotherapists and occupational therapists, and piloted at the Geriatric Day Hospital and at some of the wards. They have since been integrated into everyday care within inpatient and outpatient settings at CGH, thereby enhancing nursing care practice.
Through programmed activities and conversations in four different languages, social robots stimulate cognitive functions such as memory and problem-solving, while encouraging physical movement through guided exercises. These robots not only supplement traditional care but also provide companionship and engagement, thereby enriching the hospital experience for senior patients.
Robotic pet therapy and simulated presence therapy are other innovative approaches enhancing senior care at CGH. These technologies provide emotional support and companionship, alleviate stress and promote relaxation, especially benefiting patients with cognitive impairment.