Changi General Hospital will NEVER ask you to transfer money over a call. If in doubt, call the 24/7 ScamShield helpline at 1799, or visit the ScamShield website at www.scamshield.gov.sg.
Uncovering skeletons: Osteoporosis
We look at this condition — that affects 59% of adults aged over 60 in Singapore — which makes bones more fragile and prone to breakage.


Imagine your bones as the pillars of a building, providing support and strength. If these pillars start losing their density and become sponges that are full of holes, it is akin to getting osteoporosis, a skeletal disease in which bone density and quality are reduced. “Osteoporosis, which literally means ‘bones with holes’, is a chronic condition where bone density and quality are reduced,” explains Dr Terry Teo, Consultant, Department of Orthopaedic Surgery, Changi General Hospital (CGH). “It is often called the ‘silent disease’ as unrecognised or untreated osteoporosis increases the risk of spine or hip fractures.”
However, osteoporosis is preventable and treatable. The key is to build a strong skeleton when you are young, which will help to decrease the rate of bone loss as you age.
Identifying the risk
Certain factors increase the risk of osteoporosis. It is advisable for men aged 65 and above, post-menopausal women, and women with early menopause to go for screenings for osteoporosis. During menopause, oestrogen levels drop quickly, which can lead to reduced bone density. Persons with a family history of osteoporosis and fragility fractures, as well as those who experience a height loss of over 2cm within three years, also face an elevated risk of osteoporosis.
How does osteoporosis occur?
In adulthood, our body naturally removes old, damaged bone and replaces it with new bone every 7 to 10 years. This is known as bone remodelling.
Before 30 years old
Our bone removal rate is less than or equal to the replacement rate.
After 30 years old
Our bone removal rate is higher than the replacement rate.
Other factors that can also lead to lower bone density and the resulting osteoporosis are diabetes, inflammatory joint disease, thyroid conditions, liver diseases, renal diseases and medications such as long-term steroids.
Modifiable lifestyle factors such as inactivity, poor nutrition, low vitamin D, low calcium intake, smoking and excessive alcohol intake can also contribute to osteoporosis.
Detecting the density
Early identification of patients at risk is key. A common method to diagnose osteoporosis is through bone mineral density (BMD) testing, which uses special X-rays to determine bone density. If there are other suspected causes, blood tests may be conducted, while X-rays may be used to detect fractures.
Bridging the gaps
Healthy lifestyle choices can help reduce the risk of osteoporosis. These include weight-bearing, muscle-strengthening, and balance exercises such as walking, elastic band exercises and Tai Chi. Besides smoking cessation and appropriate alcohol intake, an appropriate calcium intake of 1,000 mg/day for healthy adults 51 years and older, and 800 mg/day for adults 19 to 50 years old can also reduce the risk of osteoporosis.
In addition, vitamin D helps the body absorb and use calcium, which strengthens the bones. Vitamin D can be found in eggs, cow or fish liver and oily fish. Other sources include fortified food products such as milk, soya milk, yoghurt, orange juice, breakfast cereals and margarine.
The daily recommended dietary allowance of vitamin D for those aged 18 and above is 2.5 micrograms (mcg) per day. One large egg yolk contains 1.02 mcg of vitamin D, and one 250 ml cup of fortified milk contains 2.9 to 3.1 mcg. Sun exposure of five to 30 minutes twice a week also helps with vitamin D intake.
What to avoid:
- Smoking
- Excessive intake of alcohol
- Very high-fibre diets
- High sodium intake
- High caffeine intake

Osteoporotic spinal fractures
Fractures caused by osteoporosis most often occur in the spine. Known as osteoporotic spinal fractures, these occur when the bones of the spine crack or break. This in turn leads to not only severe back pain that makes it difficult to stand walk, sit, or lift objects, but also a resulting humpback.
When one turns or changes positions, the pain might worsen, and in severe cases, it may result in nerve compression. When a nerve is pinched due to excessive pressure, it can cause pain, numbness or tingling in the area supplied by the nerve and may even radiate down the back of the legs. Physical examinations, magnetic resonance imaging (MRI) and X-rays are used to detect these spinal fractures.

Surgical restoration
Surgical options like kyphoplasty can help patients with osteoporotic spinal fractures. It is a minimally-invasive procedure used to treat vertebral compression fractures by inflating a balloon to restore bone height then injecting bone cement into the vertebral body.

Most osteoporotic spinal fractures can be treated without surgery. With rest, pain relief medication and wearing a brace to reduce motion in the fractures, many patients are able to recover. On the occasions when the condition does not improve, surgery might be required. The surgery serves to reduce pain, resolve the nerve compression and prevent deformities. Two common procedures are surgical fixation — which uses implants to hold the spine in position for the fracture to heal, and cement augmentation — where bone cement is injected into the fracture to reduce the compression.
“Preventing the onset of osteoporosis is the best approach,” says Dr Teo. “While there are ways to treat the condition, there are changes we can make in our lifestyle to reduce the risk of having osteoporosis, removing a major cause of disability among seniors.”

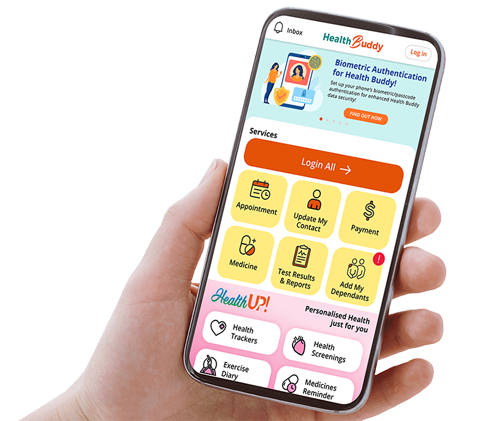
As part of CGH’s ongoing efforts to care for patients with diseases and disorders of the spine, spinal cord and nerves, the one-stop multi-disciplinary CGH-NNI Integrated Spine Centre was launched to provide comprehensive and focused care for patients.
Stay Healthy With
© 2025 SingHealth Group. All Rights Reserved.