Changi General Hospital (CGH) helps patients with obesity hypoventilation syndrome (OHS) and advanced chronic obstructive pulmonary disease (COPD) get back on their feet with a new home-based ventilation pilot programme.

With the Changi Home NIV Programme, patients living with OHS and advanced COPD now have better access to CGH’s home-based chronic NIV treatment.
Meet Mr Abu Baker Bin Mohamed Tahir, a 63-year-old who has been living with OHS since 2018. For years, he did not undergo treatment and continued to grapple with shortness of breath, disrupted sleep, heavy snoring and constant daytime sleepiness.
In June 2023, Mr Abu Baker’s sleep and respiratory condition took a severe turn when he fell ill with an Influenza A viral infection while overseas. His breathing deteriorated, leading to a nine-day admission at CGH for respiratory failure, including time in a high dependency ward for acute non-invasive ventilatory support.
It was during this challenging period that Mr Abu Baker was introduced to an innovative home-based model of care for chronic Non-Invasive Ventilation (NIV) to better address breathing difficulties and challenges faced by patients living with OHS and advanced COPD.
The pilot Changi Home NIV Programme — the first-of-its-kind in Singapore’s public hospitals — enables these patients with complex medical needs to sleep and breathe better at night, and take steps towards regaining mobility and independence.
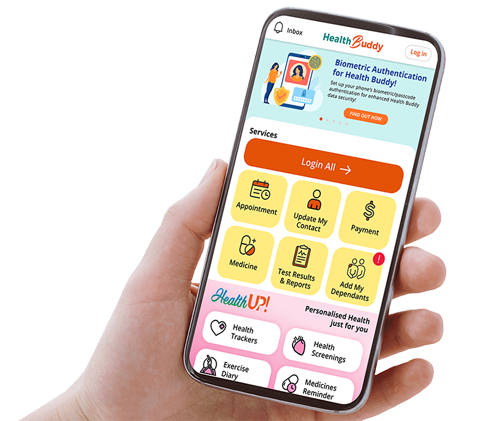
With the use of advanced ventilator technology, remote monitoring and teleconsultation, the new model of care driven by a multi-disciplinary care team at CGH aims to transform patients’ treatment experience from hospital to home, increase patient care access to NIV treatment and enhance patients’ quality of life.

“Over the years, we have become increasingly aware of the various challenges faced by OHS and COPD patients and their caregivers during treatment,” says Clinical Assistant Professor Wong Hang Siang, Chief and Senior Consultant, Department of Sleep Medicine, Surgery & Science, CGH. “If left untreated, OHS and COPD patients may face a downward spiral as their breathing difficulties and sleep disorders start to impact their lives even when awake. For instance, they may feel sleepy or drowsy all the time, breathless, moody, and are not able to lie down comfortably.” Dr Wong adds that some patients may also suffer from increased mental distress, as they are not able to work and carry out activities of daily living.
In the following weeks and months after enrolling in the programme, Mr Abu Baker, who works long hours in customer service at an MRT Passenger Service Centre, experienced a significant improvement in his condition. “The home-based ventilation treatment has greatly improved my life — both for sleep and during the day. My sleeping and breathing habits have improved, and I no longer feel breathless,” he shares. “I am also able to walk further distances both at work and for leisure, which I was never able to before.”

An innovative model of care for patients

Due to its challenges and
complexities, patients who are
unable to comply with NIV
treatment face higher chances
of hospital readmissions.
For individuals like Mr Abu Baker who battle OHS and advanced COPD, the NIV treatment is usually complex, and patients have to get accustomed to wearing the NIV mask during their sleep or treatment.
Traditionally, patients commencing NIV treatment often have to make frequent hospital visits for clinical reviews during the acclimatisation process, which includes regular adjustments on their fixed-pressure ventilator device so that they can benefit optimally from it. This poses a challenge to those with mobility issues as special transport arrangements have to be made, often by their caregivers, causing disruptions to their daily routines and work.
For those who are unable to do so, the acclimatisation process becomes less than optimal, often leading to poor treatment tolerance — such as not being able to tolerate wearing the ventilator mask or the air pressure levels — and non-compliance to treatment. Consequently, these patients are at high risk of acute respiratory failure events such as severe breathlessness. These in turn often result in hospital readmissions, which may require treatment at high dependency wards or the intensive care unit.

“As the smart and caring general hospital, CGH introduced the pilot home-based NIV treatment programme to address prevailing challenges faced by OHS and advanced COPD patients, and enhance health outcomes and patient safety,” says Clinical Assistant Professor Mok Yingjuan, Senior Consultant, CGH Department of Sleep Medicine, Surgery & Science, and the lead of the pilot programme. “Patients can receive high-quality care and support in the comfort and convenience of their homes, improve their quality of life, reduce the need for frequent hospital visits, and lower their risk of hospital readmissions.”



Chronic obstructive pulmonary disease (COPD) refers to a group of diseases that cause airflow blockage and breathing-related problems, such as emphysema and chronic bronchitis. Like OHS, COPD makes breathing difficult for patients, and is a condition associated with high rates of hospital readmission.

Obesity hypoventilation syndrome (OHS) is a life-threatening sleep-breathing disorder characterised by respiratory failure, and is associated with significant morbidity and mortality, recurrent hospitalisations and a poor quality of life. Patients with OHS experience severe breathing difficulties both during sleep and while awake in the daytime.
Complementing the home-based model of care, the programme makes use of advanced ventilator technology and remote monitoring, transmitting patient treatment data such as daily usage and air pressure requirements directly to the clinical team. Sleep specialists are able to adjust a patient’s NIV device remotely, eliminating the need for patients to make frequent hospital visits for this purpose.

The CGH multi-disciplinary team, comprising respiratory sleep physicians, sleep technologists and community nurses, supports the patients on the home-based treatment.
“We leverage the use of technology for remote monitoring, and conduct nursing assessments and health coaching for patients to ensure that they are on track with their treatment plans,” says Ms Tan Poh Choo, Assistant Director of Community Nursing, CGH.
In the ongoing pilot, the CGH team of sleep specialists has seen promising early results in the patients enrolled in the programme so far. Some patients reported being able to walk further distances and have thus regained independence. They are able to sleep without feeling breathless and experience increased energy levels upon waking up. Some patients have also been gradually weaned off oxygen support.
The pilot programme was introduced by the Changi Sleep and Assisted Ventilation Centre at CGH. The Changi Sleep and Assisted Ventilation Centre is one of the largest sleep centres in Singapore dedicated to the management of sleep disorders, promotion of sleep health and research. The Centre is run by the CGH Department of Sleep Medicine, Surgery & Science, which is recognised as a top specialty globally by Newsweek for its clinical work and research health.
No weigh to live
In conjunction with World Sleep Day on 15 March this year, learn more about a lesser-known but life-threatening sleep disorder — obesity hypoventilation syndrome (OHS).

OHS is a complex sleep disorder that affects individuals with severe obesity. Characterised by shallow breathing or pauses in breathing during sleep, OHS can have serious implications for both physical and mental health.
Understanding and treating OHS
Obese individuals with a body mass index (BMI) of 30 and above are at risk of developing OHS. The excess weight puts pressure on the chest and abdomen, making it difficult for respiratory muscles to function properly during sleep. This leads to insufficient oxygen and abnormally high levels of carbon dioxide in the blood.
Common symptoms of OHS include daytime sleepiness, fatigue, morning headaches, difficulty concentrating and shortness of breath. Left untreated, OHS can increase the risk of serious health complications such as heart disease, stroke and diabetes. OHS patients are also at high risk of recurrent hospitalisations for acute episodes of respiratory failure, which may require ventilatory support in the high dependency or intensive care unit. Consequently, many OHS patients experience difficulties with activities of daily living which further impairs their quality of life.
At the Changi Sleep and Assisted Ventilation Centre, a multi-disciplinary team of respiratory sleep physicians, sleep technologists, respiratory therapists, chest physiotherapists and nurses, provide holistic treatment and management of OHS.
Positive airway pressure (PAP) therapy and weight loss are the mainstay of treatment for OHS. PAP therapy involves the patient wearing a mask connected to a ventilatory device that delivers pressurised air to the airway during sleep. This helps to prevent airway collapse and improves ventilation and oxygen levels during sleep, thus reducing the risk of respiratory complications. Weight loss can be achieved through lifestyle modifications such as diet and exercise. Medications and surgery for weight loss may also be recommended for some patients.

Assisted ventilation during sleep is an oft-prescribed treatment option for those with OHS.
The impact on sleep and mental health
OHS not only affects sleep and breathing but can also have a significant impact on mental health and well-being. Poor sleep quality due to OHS can lead to irritability, mood swings and cognitive impairment, while the chronic stress of living with a sleep disorder can affect daily functioning and quality of life. Studies have shown that up to 50% of individuals with OHS experience symptoms of depression, anxiety or other mood disorders.
By managing OHS with appropriate treatment strategies, individuals can experience improvements in sleep quality, daytime symptoms and overall well-being. Regular follow-up appointments are essential for monitoring treatment effectiveness, adjusting ventilator therapy settings as needed and providing ongoing support.
With advancements in PAP device technologies and weight-loss strategies, individuals living with OHS can take control of their health, improve their sleep, and enhance their overall quality of life and mental well-being.