A collaboration by CGH and A*STAR on an optical wearable medical sensor was recognised at President’s Science and Technology Awards 2024.
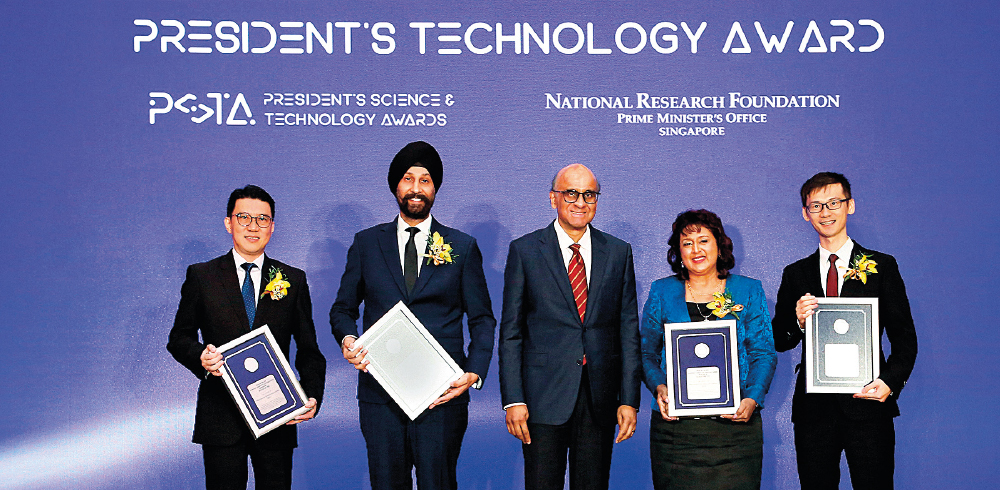
Adj Assoc Prof Augustine Tee, Dr Gurpreet Singh, President Tharman Shanmugaratnam, Prof Malini Olivo and Dr Renzhe Bi at the President’s Science and Technology Awards 2024.
CGH continues to make waves in transforming the future of healthcare — this time, for its wearable medical sensor to accurately and remotely monitor vital signs, developed in collaboration with A*STAR.
Adj Assoc Prof Augustine Tee, former Chairman, Division of Medicine and Senior Consultant, Respiratory & Critical Care Medicine, CGH; and A*STAR partners Prof Malini Olivo, Dr Gurpreet Singh and Dr Renzhe Bi were lauded for the groundbreaking device at the President’s Science and Technology Awards (PSTA) 2024. They were conferred the President’s Technology Award for their innovative integration of biophotonics, machine learning and clinical data to create the wearable medical sensor, a healthcare solution which could revolutionise cardio-respiratory disease management.
The PSTA is Singapore’s highest accolade for research scientists and engineers who drive transformational change through advancements in science and technology. It is a testament to CGH’s passion and excellence in advancing patient care and innovating healthcare for enhanced patient outcomes.
Saving time for efficient, focused care
The respiratory rate is a vital sign routinely monitored in healthcare, as respiratory rate changes are often the earliest indicator of patient deterioration.
In a general ward, nurses measure a patient’s vital signs, including some or all of the following parameters like heart rate, respiratory rate, oxygen saturation, blood pressure and temperature. The monitoring frequency varies according to a patient’s clinical needs, and it is a laborious process, as nursing staff need to manually acquire the readings at the bedside.
“Automated, reliable and continuous measurement of breathing will help healthcare professionals gain a more accurate and timely understanding of a patient’s condition, improving healthcare delivery,” explains Adj Assoc Prof Tee.
A prototype of the sensor was developed in 2018. Attached to patients’ chests, the nifty device continuously captures the respiratory rate, heart rate and oxygen saturation levels. Real-time data is then transmitted to a central system, which is displayed on a ward dashboard for nurses to monitor and to take action when needed.
Nurses can view patients’ vital signs and trends at a glance while at the nurses’ station.
The device is easily attached to the patient for monitoring.
“The monitoring process with the sensors allows nurses to focus more on engaging patients in the areas of patient education and caregiver training, that are meant to empower the patients to recover well once they are discharged,” shares Pearlyn Tan, Nurse Clinician, CGH. “Our patients can also rest undisturbed, and with the assurance that their vitals are monitored.”

Adj Assoc Prof Augustine Tee and the A*STAR team focused on the development of a wearable sensor that would meet stringent clinical needs in its early phase of development. (Credit: National Research Foundation Singapore)
From idea to reality
CGH kickstarted the clinical validation trial for the wearable sensors at two COVID-19-related facilities in 2020 amid the pandemic, placing the devices on patients who were diagnosed with respiratory tract infection. The sensor’s remote detection of vital signs provided frequent, accurate data to the care team while minimising their risk of potential exposure to infectious diseases.
The medical sensor was clinically validated at CGH, and the team is now leveraging AI to further augment device capabilities.
To demonstrate real-world viability of the wearable technology, the CGH care team, supported by the CGH Office of Innovation, continued to conduct patient trials to validate its use, refining and guiding the enhancement of the sensor. “This ensures that the medical device can provide the accuracy that is expected for vital signs monitoring, and meet the stringent clinical and patient safety standards for use in hospital settings,” adds Dr Aza Taha, Senior Consultant, Department of Respiratory & Critical Care Medicine, CGH. This also allowed for the subsequent scaling and licensing of the technology, and the optical wearable technology has since received global and local regulatory clearances and patent grants.
The team is now leveraging artificial intelligence (AI) to augment this remote monitoring device with diagnostic and predictive capabilities. The technology’s predictive AI algorithm — developed and validated in continued collaboration with A*STAR — has exhibited the capacity to predict patient deterioration, providing a lead time of 18-21 hours prior to the manifestation of deterioration at a performance of 91.7%. “This will facilitate early alerts of patient deterioration and signal for the care team’s quick intervention for improved patient outcomes,” says Adj Assoc Prof Tee.

